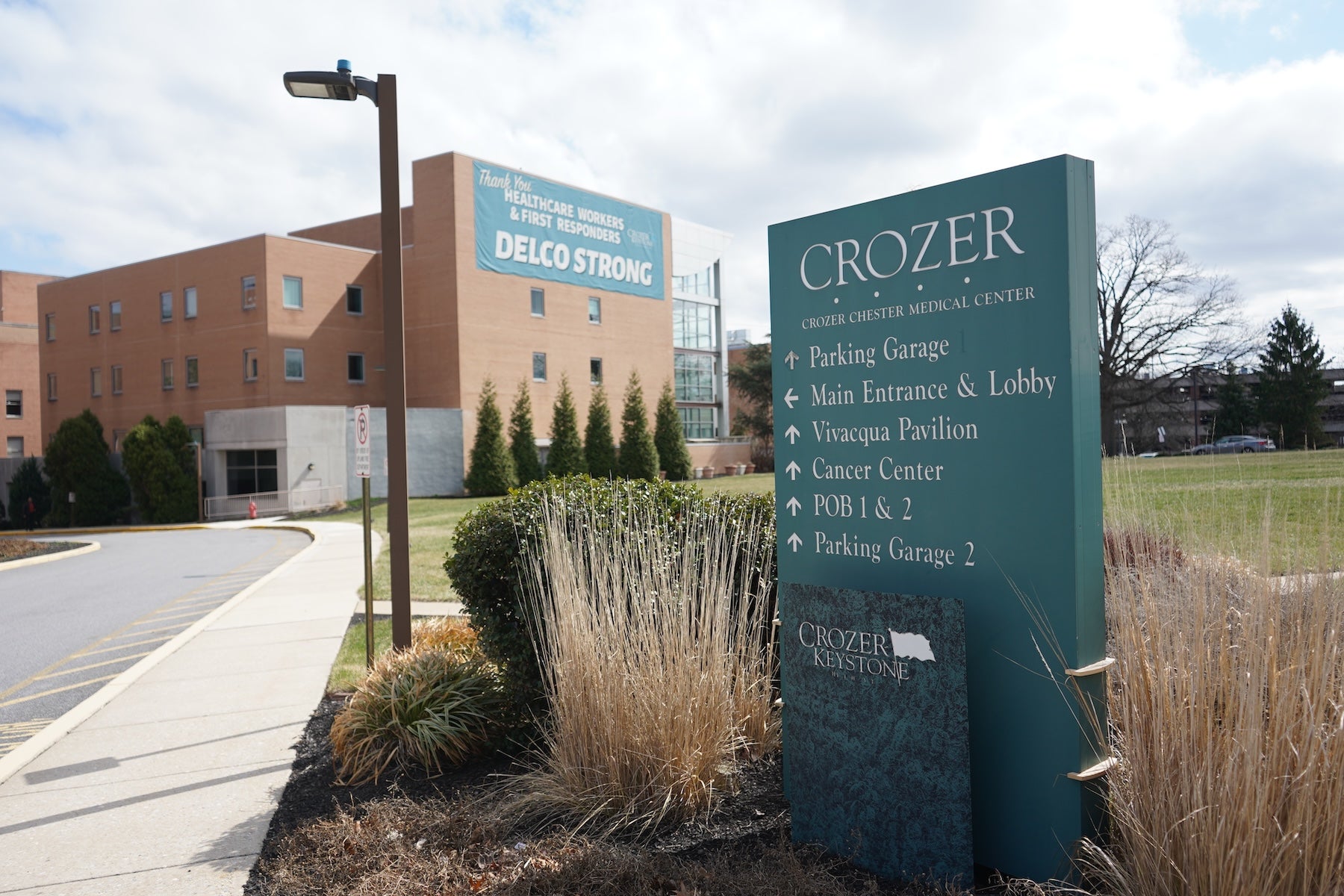
Healthcare Showdown: Prospect Threatens to Shutter Crozer Health Without Urgent $9M State Lifeline
Facing a critical financial crossroads, the hospital system is on the brink of implementing emergency measures. Without a crucial cash infusion by Wednesday, administrators are preparing to redirect ambulances and redirect patient care to alternative medical facilities as early as Thursday morning. This potential redirection could significantly impact emergency medical services and patient access to healthcare in the region, highlighting the urgent financial challenges confronting the medical institution.
The looming possibility of diversion underscores the system's precarious financial situation, potentially forcing patients to seek treatment at other hospitals and potentially disrupting established medical care networks. Healthcare leaders are racing against the clock to secure the necessary funding and prevent a potentially disruptive operational shift that could compromise patient care and community health services.
