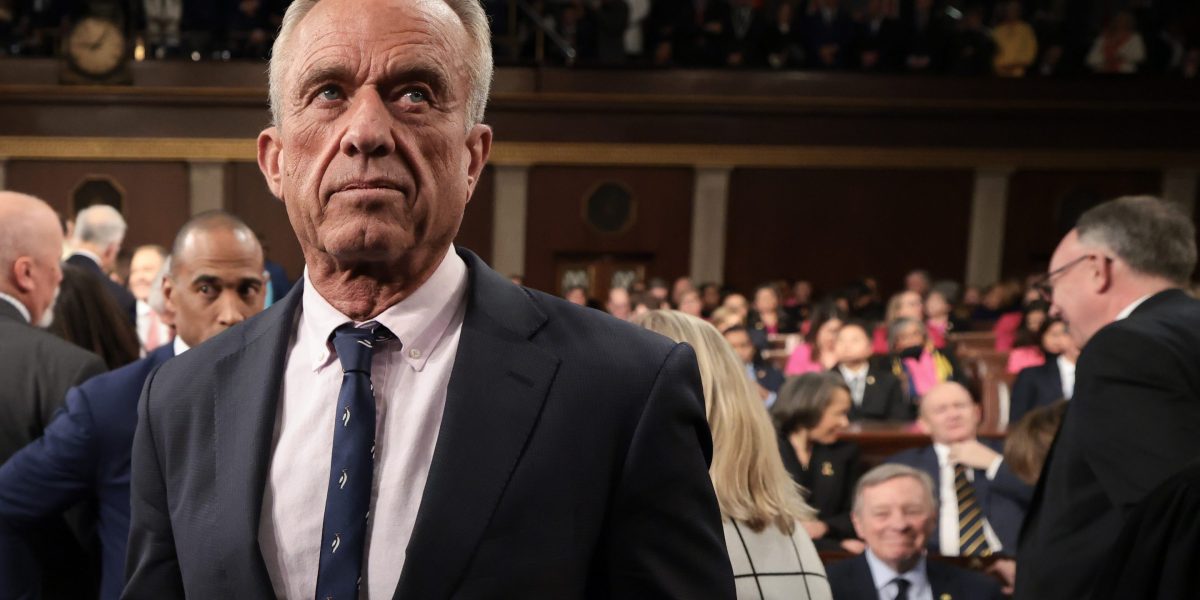
Wealth Erosion: RFK Jr.'s Controversial Plan Threatens Long-Term Economic Stability
Experts unanimously agree that the Trump administration has inflicted significant and lasting harm in one critical domain: public health. The impact of policy decisions and administrative actions during this period has raised serious concerns among healthcare professionals and policy analysts about the long-term consequences for the nation's medical landscape.
The administration's approach to public health challenges has been marked by controversial strategies that have potentially undermined critical healthcare infrastructure, research funding, and pandemic response mechanisms. These actions have not only created immediate challenges but also potentially compromised the resilience and preparedness of the United States' healthcare system for future health crises.
