Uncertain Future: Crozer Health Shutters Doors, Leaving Patients and Staff in Crisis
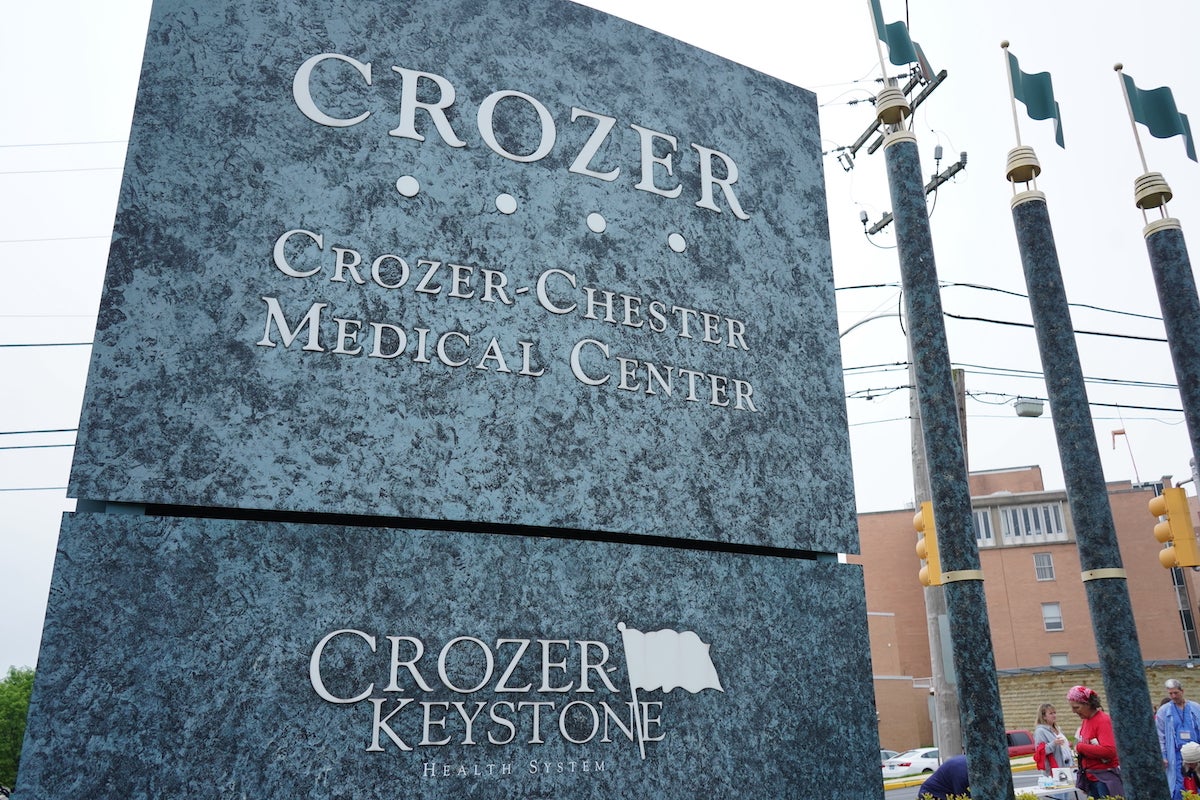
In a dramatic move that will significantly impact healthcare services in Delaware County, Prospect Medical Holdings, a for-profit parent company, announced on Monday its intention to close the region's largest hospital system. The decision sends shockwaves through the local community, raising serious concerns about medical access and healthcare infrastructure for thousands of residents.
The sudden closure highlights the growing challenges faced by regional healthcare providers, particularly those under the ownership of private equity firms. Prospect Medical Holdings' decision underscores the complex and often unpredictable landscape of modern healthcare management, where financial considerations can swiftly reshape critical medical services.
Local officials and community leaders are scrambling to understand the full implications of this unexpected shutdown, with many expressing deep worry about the potential gaps in medical care that may emerge in the wake of this announcement. Patients, healthcare workers, and local residents are left uncertain about the future of their medical services and the broader healthcare ecosystem in Delaware County.
