Healing on the Brink: NH's Health Centers Struggle with Staffing Shortage
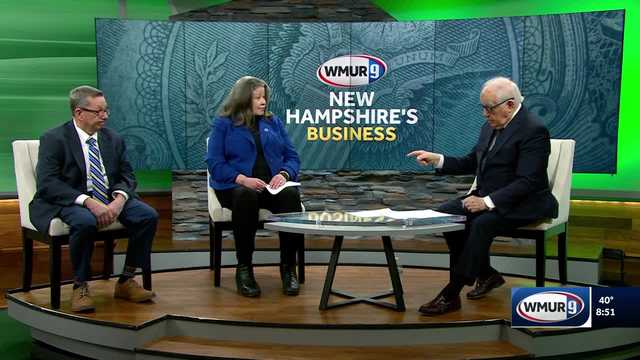
In a candid conversation with Fred Kocher, two healthcare leaders from New Hampshire shed light on the critical challenges facing community health centers. Kris McCracken, CEO of Amoskeag Health, and Robert MacLeod, CEO of Mid-State Health Center, voiced their deep concerns about proposed budget cuts that threaten to further strain already struggling medical facilities.
The discussion highlighted the mounting pressures on community health centers, which are grappling with significant financial constraints and workforce shortages. These vital healthcare providers serve as lifelines for many communities, offering essential medical services to vulnerable populations who might otherwise lack access to quality healthcare.
McCracken and MacLeod emphasized the potential devastating impact of these budget cuts, warning that they could compromise the ability of community health centers to provide critical medical services. Their passionate plea underscores the urgent need to protect and support these essential healthcare institutions that play a crucial role in maintaining the health and well-being of local communities.
