Breaking: Sacramento's Bold Move to Slash Healthcare Bureaucracy
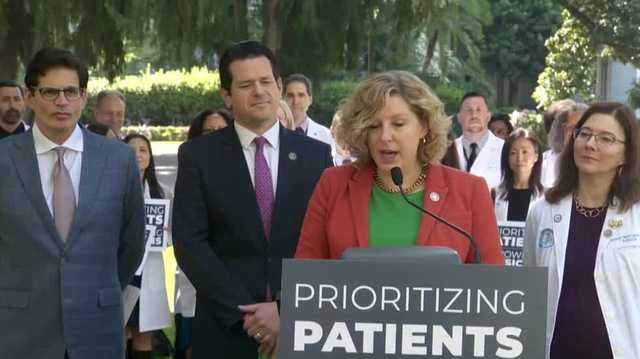
Advocates for the proposed legislation are championing a critical reform that targets the often frustrating healthcare practice of prior authorization. This complex process currently forces physicians to navigate a bureaucratic maze, requiring them to obtain explicit approval from health insurance providers before delivering essential patient care.
The bill package seeks to streamline and simplify this administrative hurdle, which has long been a source of frustration for medical professionals and patients alike. By addressing the prior authorization bottleneck, supporters hope to expedite medical treatments, reduce unnecessary delays, and ultimately improve the overall healthcare experience.
Under the current system, doctors must submit detailed documentation and wait for insurance companies to review and approve medical procedures, treatments, and prescriptions. This time-consuming process can potentially compromise patient care by creating significant barriers to timely medical interventions.
The proposed legislation aims to cut through this red tape, empowering healthcare providers to make more immediate and patient-centered decisions while maintaining appropriate oversight and cost management.
